Understanding Your Diagnoses
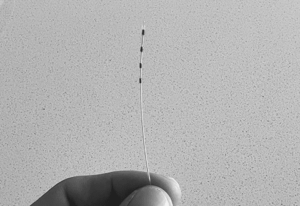
- Stellate Ganglion Block: EffectsThe most common indication for stellate ganglion block is complex regional pain syndrome of the upper extremity. Additional indications for stellate ganglion blockade include: neuropathic...
- Add to CRPSThe treatment of complex regional pain syndrome (CRPS) is centered around a multidisciplinary team-based approach to control pain and restore function. Early diagnosis and appropriate...
- Post Herpetic NeuralgiaPost herpetic neuralgia (PHN) is a sequelae of herpes zoster infection. Herpes zoster infection typically begins with flu like prodromal symptoms and progresses to a...