Functional Pain Management Procedures
- Spinal Cord StimulationSpinal cord stimulation or “SCS” offers a non-opioid, FDA-approved alternative for chronic pain treatments when other therapies such as physical therapy, medication, injections, or surgery...
- At Home Temporary SCS SystemThe SCS trial lasts anywhere from 5 days to 14 days, depending on what your doctor decides is best for you. During the trial, consider...
- Radiofrequency AblationThis procedure uses cooled radiofrequency energy through a probe to safely target the sensory nerves responsible for sending pain signals. A radiofrequency generator transmits a small...
- Regenerative MedicinePRP stands for platelet-rich plasma, and BMAC stands for bone marrow aspirate concentration. This therapy may be used to treat various acute and chronic pain...
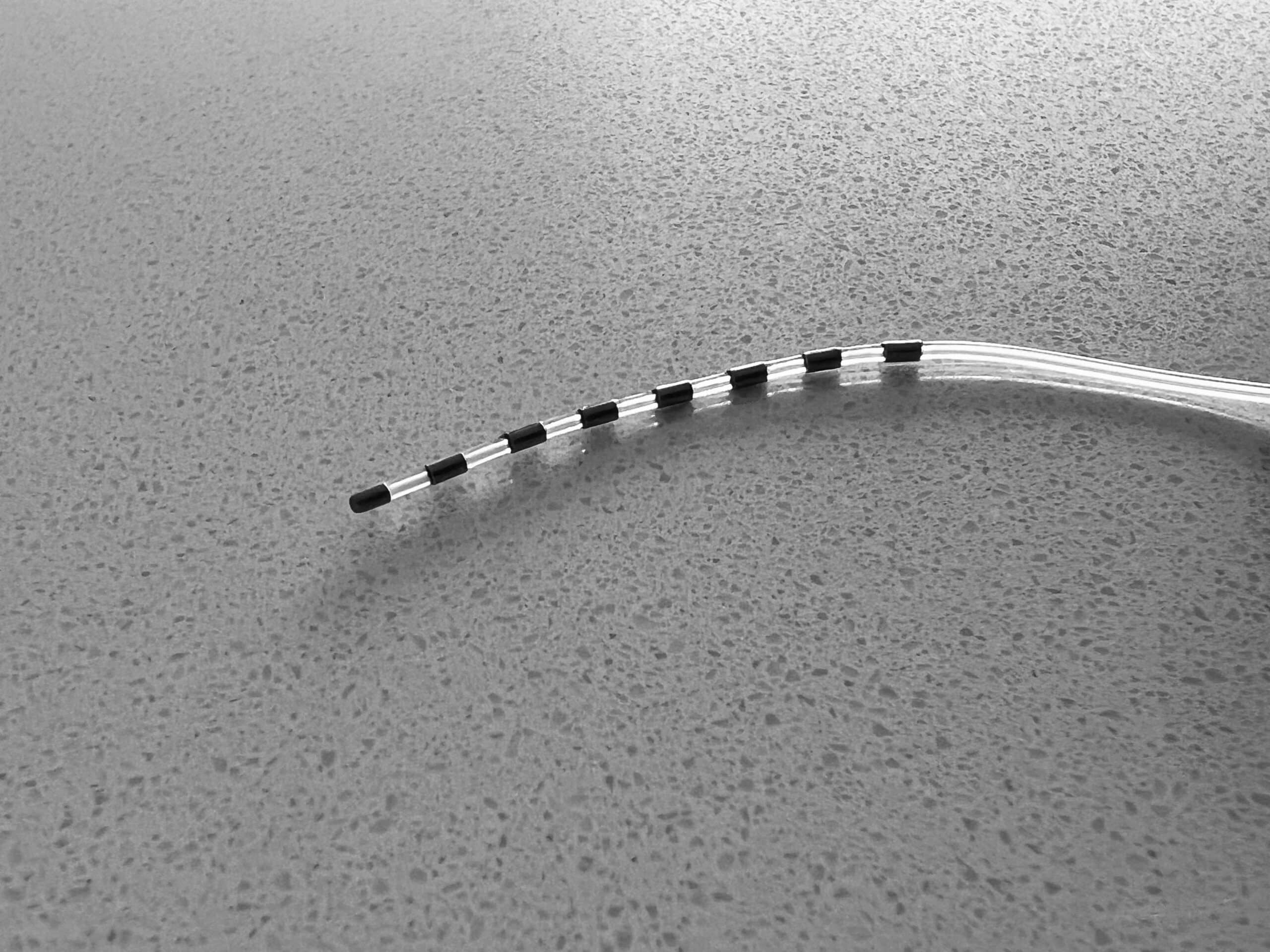
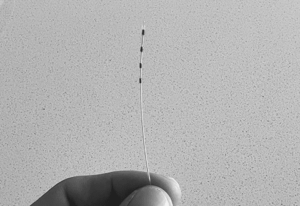
- Peripheral Nerve StimulationPeripheral Nerve Stimulation provides long lasting pain relief by blocking pain signals from reaching the brain. Nerve related pain is blocked by delivering a week...
- Intrathecal Drug DeliveryTargeted drug delivery is a safe and effective way to manage chronic pain or cancer pain with fewer side effects and lower drug doses compared...
- Indirect Spinal DecompressionLumbar spinal stenosis is when there is a narrowing of the spinal canal due to degenerative changes in the spine. The narrowing may cause pain,...
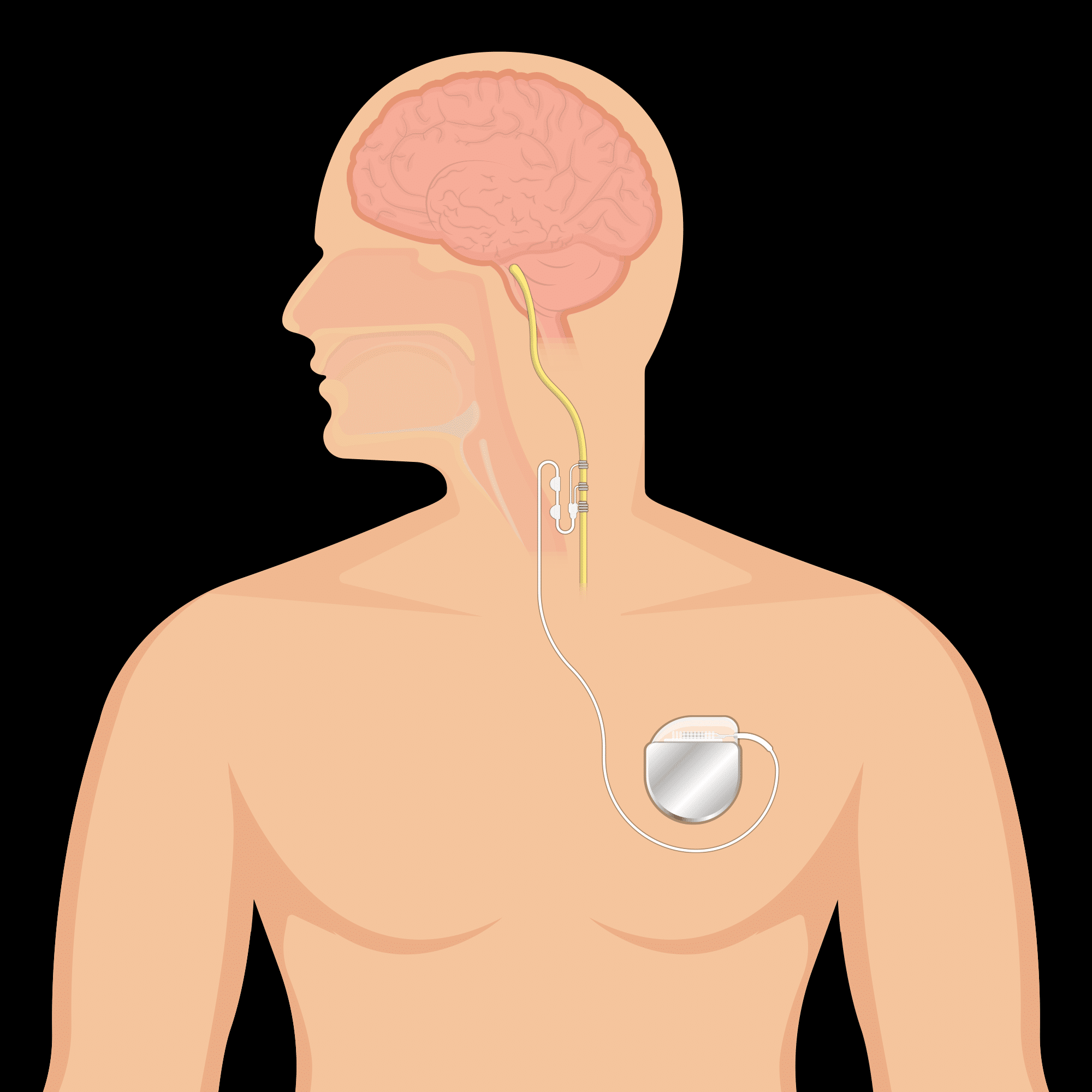
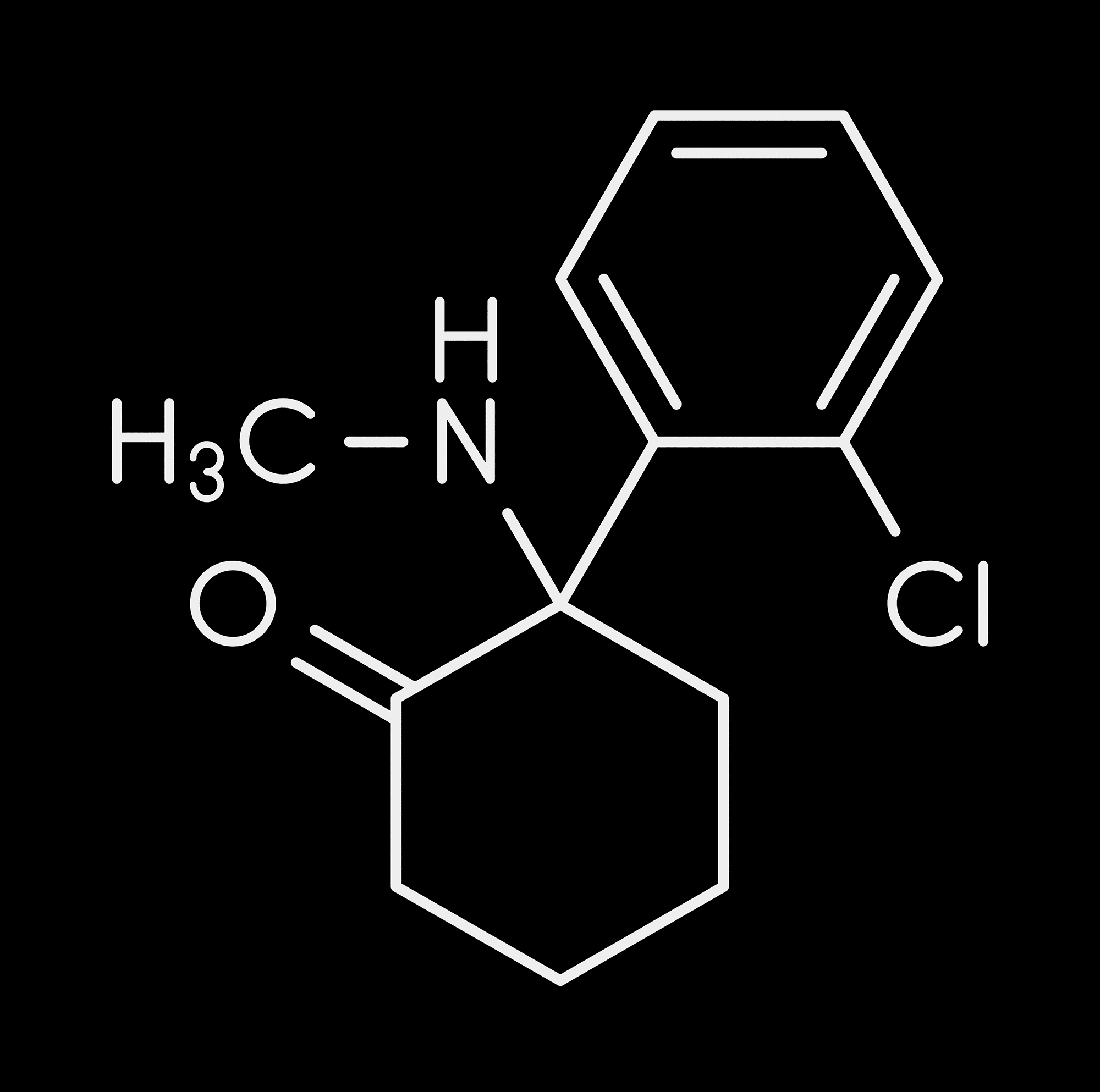
- KetamineThe action of ketamine involves multiple mechanisms with multiple receptors. Ketamine is noncompetitive, reversible N-methyl-D-aspartate (NMDA) channel blocker which blocks the excited nerves, potentiates delta...
- Phantom Limb PainPost-amputation pain (PAP) is a challenging constellation of painful disease states caused by the surgical or traumatic removal of a limb or appendage. The most...